The Blue Zones Debunked (Again)
The field of nutrition is always very exciting. We have documentaries, studies, guidelines, etc. coming out on a regular rhythm often with polarizing subjects: the Blue Zones, meat causes heart disease, everyone including those with diabetes should eat 45-65% of your calories from carbohydrates are some of these topics. The Blue Zones is an interesting look at cultures that live long and healthy lives. It’s essentially one author’s interpretation of what makes the Blue Zones healthy for those that live there.
It unfortunately has zeroed in on a plant-based diet, when in reality there is a plethora of other very important factors like consistent low stress, lots of daily movement, strong social connections and more. PLUS there is the fact that the author, Dan Buettner, omitted cultures that live even longer with healthy lifespans like Hong Kong in order to promote a plant-based diet. He even tweaked diets like the Okinawans to seem more plant-based then they actually were.
You can read about my examination of that here.
This is extremely frustrating because even though the plant-based diet is touted as the gold standard of all diets, it has many overlooked flaws. It leads to nutrient deficiencies (iron, protein, omega 3, zinc, B12, creatine), vegan diets are often high in processed foods and high in pro-inflammatory vegetable oils, they are not very filling or satisfying for most people and they are not more heart healthy or better for the planet.
Ooof…. I said a lot of things that go against the conventional narrative. Here is where I see why we are in this dire situation and yes, it has a lot to do with the bad information we are given. Our culture is obsessed with the latest “health” information, yet almost every single American is metabolically unhealthy.
Why? Based on my clinical experience, junk food bombards us everywhere and our national nutrition guidelines (USDA MyPlate) cause dissatisfaction. It promotes the majority of calories from high carbohydrates especially grains. The high carbohydrate intake perpetuates blood sugar spikes and crashes, causing cravings. It shys away from animal fat and promotes a generally low-fat diet with an emphasis of “vegetable” seed oil. Low fat diets are unsatisfying which leads to snacking, binging and junk food.
Plant-based dairy, cheese, “meat” alternatives are highly, highly processed and are often GMOs and from mono crop farming. Corn, soy and wheat fields are not naturally formed in nature which is why the tend to require intensive watering, pesticides and herbicides. And in case you didn’t know, our pre-species and species has eaten meat for 3.5 million years; we need to eat meat - with the protein and fat - to be satisfied.
Seeds oils are now being shown to cause insulin resistance in fat cells. Seed oils were only introduced into the diet the last 100 years and intake has skyrocketed to the primary fat source, replacing butter, lard, tallow. It’s also an extremely processed food.
Why would our national guidelines do this? There unfortunately tons of conflicts of interest from Big Food and Big Pharma (read + read) vested in addicting us to junk food and making us sick. The US allows businesses to lobby the government, it permits business executives to run for office, it allows businesses to give money to campaigns, stocks for promises and promotion. 95% of the USDA MyPlate committee members had COI with the food, and/or pharmaceutical industries. You name it, it’s happening. Just follow the money.
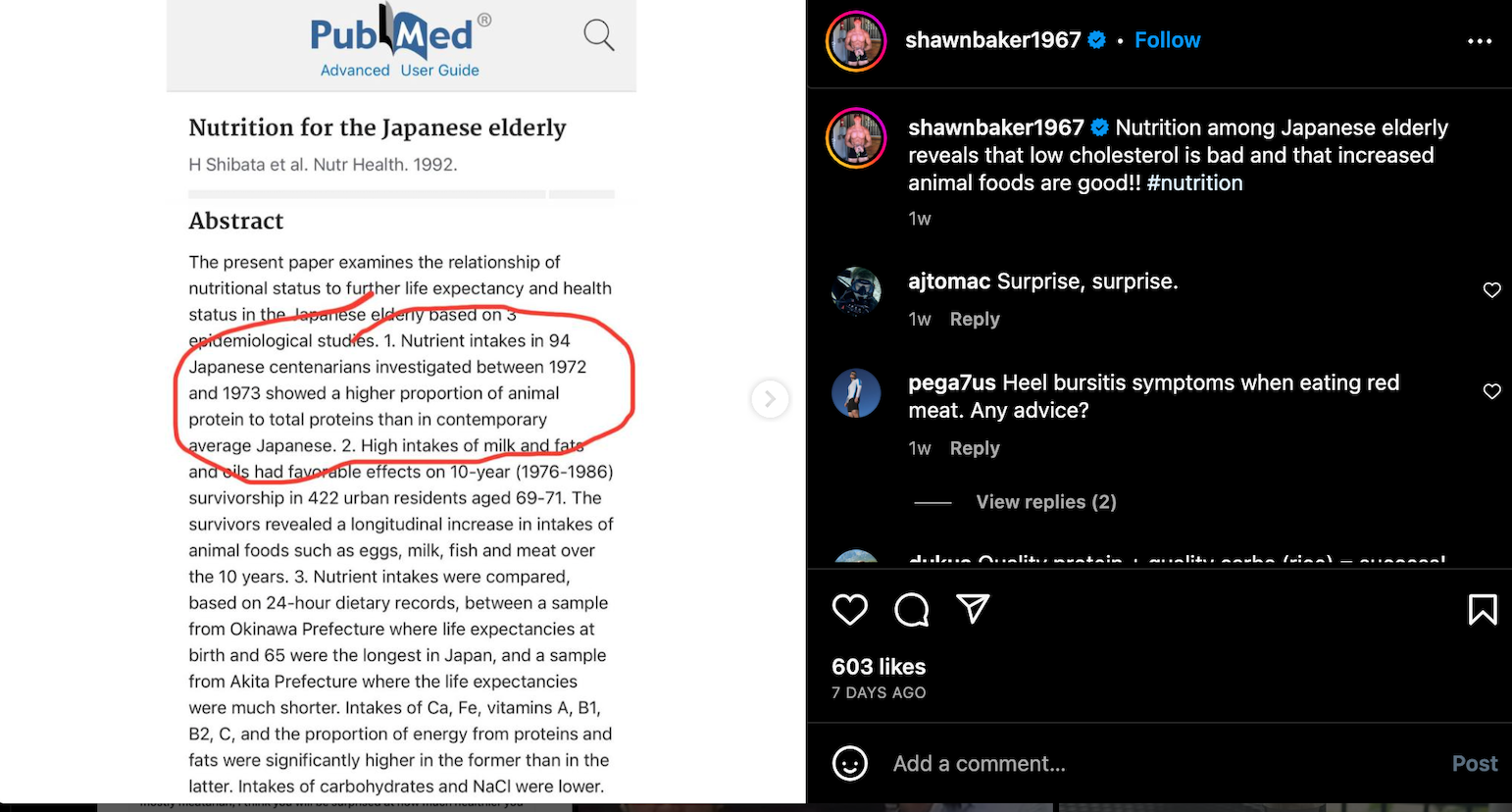
So it’s no surprise to see that now the USDA MyPlate came up with a study that says you can eat a 90% processed food diet and still get the plant-based nutrition you need. Isn’t this just bonkers?! Many, many studies in the last 10 years have started not only questioning but calling for a change in the “red meat/animal fat is bad” propaganda. At the bottom I have compiled a list of some of those studies plus a well-written article by Chris Kresser here.
All the finger pointing at meat is criminal. 100% pasture-raised meat is wonderful for health and the planet. Study after study is sounding the alarm that all this meat hate will be detrimental to our health.
The role of meat in the human diet: evolutionary aspects and nutritional value: Aspects of human anatomy, digestion, and metabolism diverged from other primates, indicating evolutionary reliance on, and compatibility with, substantial meat intake. Implications of a disconnect from evolutionary dietary patterns may contribute to today’s burden of disease, increasing the risk for both nutrient deficiencies and chronic diseases. As a food matrix, meat is more than the sum of its individual nutrients. Moreover, within the diet matrix, it can serve as a keystone food in food-based dietary interventions to improve nutritional status, especially in regions that rely heavily on cereal staples.
Further, a cow eating on a pasture is grazing in a natural habitat and is also improving the plant ecosystem and helps capture even more carbon out of the atmosphere. Unfortunately, the the study that is often used in terms of beef being water intensive compared to plant foods is highly inaccurate as outlined in this podcast.
Lastly, we cannot simplify foodstuffs as good or bad based on how much water they need or carbon they emit. We need to consider our human evolution with food and nutrient density. Savvy carbon researchers are now suggesting that the full nutritional value of foodstuffs needs to be considred when scientests are trying to calculate the environmental impact of producing different foods. In a study, the authors took a measure of protein quality called the Digestible Indispensible Amino Acid Score and used it to create ‘adjusted’ environemental footprint metrics for a variety of foods. Using this method, many animal products’ environmental impacts were almost halved (dairy, beef) whilst the impacts associated with wheat bread, for instance increased by almost 60%.
In summation, pre-humans have been eating meat for millions of years. Our genetics have evolved with needing to eat meat to thrive. Often plant-based diets IE vegetarian and vegan cause multiple nutrient deficiencies. Eating meat improves satiety, muscle mass, strength and overall longevity. By eating meat, you get healthier, nourished people who avoid reliance on the medical system and the medical system is a HUGE single-use plastic and carbon polluter.
And I am not saying these things without the data to back this up. Over and over and over again my clients eat eggs, butter, steak and their biomarkers improve. Their glucose sensitivity improves, their HDL maintains or increases, their triglycerides go down and their waist measurement goes down. They feel better: full longer, less cravings and higher energy. These are not signs of a body in peril and in fact are signs that the body is finally in equilibrium.
How many studies like these do we need before the dietary guidelines in the United States are updated to reflect what the research is saying?
July 2020. Diamond et al. “Dietary Recommendations for Familial Hypercholesterolaemia: an Evidence-Free Zone.” BMJ Evidence-Based Medicine. 2020.
December 2019: Heileson. “Dietary saturated fat and heart disease: a narrative review.” Nutrition Reviews. 2019. Conclusion: The American Heart Association stance regarding the strength of the evidence for the recommendation to limit SFAs for heart disease prevention may be overstated and in need of reevaluation.
September 2019: Mozaffarian. “Dairy Foods, Obesity, and Metabolic Health: The Role of the Food Matrix Compared with Single Nutrients.” Advances in Nutrition. 2019. Conclusion: Based on the current science, dairy consumption is part of a healthy diet, without strong evidence to favor reduced-fat products; while intakes of probiotic-containing unsweetened and fermented dairy products such as yogurt and cheese appear especially beneficial.
September 2018: Gershuni V.M. Saturated Fat: Part of a Healthy Diet. Current Nutrition Reports. 2018.
September 11th 2018: Mente et al. “Association of dairy intake with cardiovascular disease and mortality in 21 countries from five continents (PURE): a prospective cohort study.” The Lancet. 2018. Conclusion: Dairy consumption was associated with lower risk of mortality and major cardiovascular disease events in a diverse multinational cohort.
August 14th 2018: Harcombe Z. US dietary guidelines: is saturated fat a nutrient of concern? Br. J. Sports Med. 2018. Conclusion: The answer is that there is adequate evidence of no relationship between saturated fat consumption during adulthood and actual CVD outcomes. There is also strong agreement from robust meta-analyses of no relationship between saturated fat consumption and: total mortality; CVD mortality; fatal MIs; non-fatal MIs; strokes; CHD mortality or CHD events.
March 26th 2018: Grasgruber P et al. “Global Correlates of Cardiovascular Risk: A Comparison of 158 Countries.” Nutrients. 2018. Conclusion: Regardless of the statistical method used, the results always show very similar trends and identify high carbohydrate consumption (mainly in the form of cereals and wheat, in particular) as the dietary factor most consistently associated with the risk of CVDs. These findings are in line with the changing view of the causes of CVDs.
January 2018: Zinn et al. “Assessing the nutrient intake of a low carbohydrate, high-fat (LCHF) diet: a
hypothetical case study design”. BMJ Open. 2018. Conclusion: Despite macronutrient proportions not aligning with current national dietary guidelines, a well-planned LCHF meal plan can be considered micronutrient replete. August 29th 2017: Dehghan et al. “Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study.” The Lancet. 2017. Conclusion: High carbohydrate intake was associated with higher risk of total mortality, whereas total fat and individual types of fat were related to lower total mortality. Total fat and types of fat were not associated with cardiovascular disease, myocardial infarction, or cardiovascular disease mortality, whereas saturated fat had an inverse association with stroke. Global dietary guidelines should be reconsidered in light of these findings.
August 24th 2017: Kelly et al. “Whole grain cereals for cardiovascular disease.” Cochrane Review. 2017. Conclusion: There is insufficient evidence from randomised controlled trials to date to recommend consumption of whole grain diets to reduce the risk of cardiovascular disease, or lower blood cholesterol, or blood pressure.
May 19th 2017: Hamley, Steven. “The effect of replacing saturated fat with mostly n-6 polyunsaturated fat on coronary heart disease: a meta-analysis of randomised controlled trials.” Nutrition Journal. 2017. Conclusion: Available evidence from adequately controlled randomised controlled trials suggest replacing SFA with mostly n-6 PUFA is unlikely to reduce CHD events, CHD mortality or total mortality. The suggestion of benefits reported in earlier meta-analyses is due to the inclusion of inadequately controlled trials. These findings have implications for current dietary recommendations.
pril 25th 2017: Malhotra, Redberg & Meier. “Saturated fat does not clog the arteries: coronary heart disease is a chronic inflammatory condition, the risk of which can be effectively reduced from healthy lifestyle interventions.” Br. J. Sports Med. 2017.
January 1st 2017: Noakes & Windt. “Evidence that supports the prescription of low-carbohydrate high-fat diets: a narrative review.” Br. J. Sports Med. 2017. Conclusion: Blood total cholesterol and LDL-cholesterol concentrations show a variable, highly individual response to LCHF diets, and should be monitored in patients adhering to this diet. In contrast available evidence from clinical and preclinical studies indicates that LCHF diets consistently improve all other markers of cardiovascular risk—lowering elevated blood glucose, insulin, triglyceride, ApoB and saturated fat (especially palmitoleic acid) concentrations, reducing small dense LDL particle numbers, glycated haemoglobin (HbA1c) levels, blood pressure and body weight while increasing low HDL-cholesterol concentrations and reversing non-alcoholic fatty liver disease (NAFLD). This particular combination of favourable modifications to all these risk factors is a benefit unique to LCHF diets. These effects are likely due in part to reduced hunger and decreased ad libitum calorie intake common to lowcarbohydrate diets, allied to a reduction in hyperinsulinaemia, and reversal of NAFLD.
October 18th 2016: Harcombe Z. “Dietary fat guidelines have no evidence base: where next for public health nutritional advice?” Br. J. Sports Med. 2016.
October 3rd 2016: Harcombe et al. “Evidence from prospective cohort studies does not support current dietary fat guidelines: a systematic review and meta-analysis.” Br. J. Sports Med. 2016.
September 27th 2016: Pavel Grasgruber et al. “Food consumption and the actual statistics of cardiovascular diseases: An epidemiological comparison of 42 European countries.” Food & Nutrition Research. 2016 Conclusion: Our results do not support the association between CVDs and saturated fat, which is still contained in official dietary guidelines. Instead, they agree with data accumulated from recent studies that link CVD risk with the high glycaemic index/load of carbohydrate-based diets. In the absence of any scientific evidence connecting saturated fat with CVDs, these findings show that current dietary recommendations regarding CVDs should be seriously reconsidered.
August 19th 2016: Unwin, Haslam & Livesey. “It is the glycaemic response to, not the carbohydrate content of food that matters in diabetes and obesity: The glycaemic index revisited.” Journal of Insulin Resistance. 2016
August 8th 2016: Harcombe et al. “Evidence from randomised controlled trials does not support current dietary fat guidelines: a systematic review and meta-analysis.” BMJ Open Heart. 2015.
June 29th 2016: Harcombe et al: “Evidence from prospective cohort studies did not support the introduction of dietary fat guidelines in 1977 and 1983: a systematic review.” Br. J. Sports Med. 2016.
June 13th 2016: Harcombe Z. “Designed by the food industry for wealth, not health: the ‘Eatwell Guide’.” Br. J. Sports Med. 2016.
March/April 2016: DiNicolantonio JJ, Harcombe Z, O’Keefe JH. “Problems with the 2015 Dietary Guidelines for Americans: An Alternative.” Mo. Med. 2016.
January 20th 2016: Jaike Praagman et al “The association between dietary saturated fatty acids and ischemic heart disease depends on the type and source of fatty acid in the European Prospective Investigation into Cancer and Nutrition–Netherlands cohort.” AJCN. 2016. Conclusion: The results we observed for SFAs differing in carbon chain length and IHD risk correspond in part with our results for SFAs from food sources. Our results suggest that the inverse association between total SFAs and IHD was mainly driven by SFAs from dairy sources.
October 20th 2015: Jonathan Sackner-Bernstein, David Kanter & Sanjay Kaul. “Dietary Intervention for Overweight and Obese Adults: Comparison of Low-Carbohydrate and Low-Fat Diets. A Meta-Analysis.” PLoS One 2015. Conclusion: This trial-level meta-analysis of randomized controlled trials comparing LoCHO diets with LoFAT diets in strictly adherent populations demonstrates that each diet was associated with significant weight loss and reduction in predicted risk of ASCVD events. However, LoCHO diet was associated with modest but significantly greater improvements in weight loss and predicted ASCVD risk in studies from 8 weeks to 24 months in duration.
August 26th 2015: Malhotra et al. “It is time to stop counting calories, and time instead to promote dietary changes that substantially and rapidly reduce cardiovascular morbidity and mortality.” BMJ Open Heart. 2015. Conclusion: Focusing on total energy consumed, as opposed to nutritional value, has been exploited by the food industry, which has added sugar to over 80% of all processed foods. One can of cola contains nine teaspoons of sugar. The EPIC study revealed that one can a day (approximately 150 calories) was associated with substantially increasing the risk of developing type 2 diabetes.21 Conversely, PREDIMED revealed that consumption of a handful of nuts, (30 g of walnuts, 15 g of almonds and 15 g of hazelnuts) or four tablespoons of extra virgin olive oil per day (approximately 500 calories) significantly reduced the risk of heart attack and stroke.
August 12th 2015: de Souza, R. J., et al. “Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies.” BMJ. 2015. Conclusion: Saturated fats are not associated with all cause mortality, CVD, CHD, ischemic stroke, or type 2 diabetes, but the evidence is heterogeneous with methodological limitations.
July 15th 2015: Tanja K Thorning et al. “Diets with high-fat cheese, high-fat meat, or carbohydrate on cardiovascular risk markers in overweight postmenopausal women: a randomized crossover trial.” AJCN. 2015. Conclusion: Diets with cheese and meat as primary sources of SFAs cause higher HDL cholesterol and apo A-I and, therefore, appear to be less atherogenic than is a low-fat, high-carbohydrate diet.
June 9th 2015: Edward Archer, Gregory Pavela, Carl J. Lavie. “The Inadmissibility of What We Eat in America and NHANES Dietary Data in Nutrition and Obesity Research and the Scientific Formulation of National Dietary Guidelines.” Mayo Clinic Proceedings. 2015. Video interview here.
May 7th 2015: Malhotra, Noakes & Phinney. “It is time to bust the myth of physical inactivity: you cannot outrun a bad diet.” British Journal of Sports Medicine. 2015.
February 9th 2015: Harcombe et al. “Evidence from randomised controlled trials did not support the introduction of dietary fat guidelines in 1977 and 1983: a systematic review and meta-analysis.” BMJ Open Heart. 2015.
February 1st 2015: Nathalie Genevieve Puaschitz et al. “Dietary Intake of Saturated Fat Is Not Associated with Risk of Coronary Events or Mortality in Patients with Established Coronary Artery Disease.” The Journal of Nutrition. (Many thanks to Ted Hutchinson for this one).
January 26th 2015: Zoë Harcombe. What caused the obesity epidemic? Trends in Urology & Men’s Health. (2015).